 |  |
| MENU Risk Factors for Transmission Occupational Risk for Nurses HIV Pathophysiology Clinical Manifestations Etiology Treatment Nursing Care Case Study |
The Basics: HIV/AIDS 101
|
 |  |
| MENU Risk Factors for Transmission Occupational Risk for Nurses HIV Pathophysiology Clinical Manifestations Etiology Treatment Nursing Care Case Study |
The Basics: HIV/AIDS 101
|
Fact: Canada tests 100% of blood products for HIV4. (Did you know less than 3.7% of people in Canada donate blood? Click here to donate!
HIV is found in blood and bodily fluids.
The following fluids contain high levels of HIV:These bodily fluids do not contain enough HIV to infect, unless: 1) They are visibly contaminated by blood; and 2) There is significant and direct contact5.
Question: What PPEs would you want to wear in each of the following nursing care activities for an HIV positive patient who is on treatment?
| 1. Giving a bed bath | ||||
| 2. Changing adult pads soiled with urine and feces | ||||
| 3. Changing linens soiled with blood | ||||
| 4. Giving an injection | ||||
| 5. Withdrawing blood | ||||
| 6. Changing a wound dressing |
The membrane lining of the anus and cervix are composed of simple columnar epithelium that are one cell layer thick thus make it easy for HIV to cross the membrane. In addition, the mucous membrane of the anus is more susceptible to tearing because it does not produce lubrication to reduce friction during sexual intercourse - making unprotected anal sexual intercourse the riskiest type of sexual behavior.6
The foreskin of the penis (the inner layer) is also a mucous membrane that is more susceptible to HIV infection. Although this area is composed of stratified epithelium with many cell layers, it has many immune cells, called dendritic cells, that HIV binds to in order to enter the body. In fact, circumcision has been found to reduce the chance of acquiring HIV by almost 50%.7
The mouth is also a mucous membrane where HIV can enter the body, although sexual intercourse still carries the highest risk for HIV infection. Factors that can increase the risk of contracting HIV through the oral mucosa include:
|
|
In a person who is HIV positive: Inflammation can increase the viral load in certain bodily fluids because inflammation activates the immune system, which causes infected CD4+ cells to produce more copies of HIV, thus increasing the viral load.
In a person who is HIV negative: Inflammation and the resulting accumulation of CD4+ cells (helper T cells) in the area will make it easier for HIV to come into contact with non-infected CD4+ cells.
Question: You are caring for a young adult who has been diagnosed with gonorrhea - a bacterial infection that is transmitted sexually and causes inflammation of the penis and vagina. Through the health history, you learn that this patient has engaged in unprotected sex with multiple partners. What patient teaching would you provide in regards to the link between sexually transmitted diseases (STDs) and HIV?
As a nurse, you recognize that IV drug users are at a higher risk for contracting HIV. Combined with a thorough health history including engagement in risky behaviors will inform you as to whether or not to refer the patient for HIV testing. Avoid stigmatization by assuming that everyone from a high risk population needs to be tested for HIV.
PPEs are usually not necessary during a health history interview. Over-protection may contribute to stigmatization of people living with HIV/AIDS by health care professionals. Consent is also necessary in order to refer a patient for HIV testing.
Go back to the question Sorry, wrong answer.Try again. :) That's correct! Good job.STDs can cause inflammation, resulting in activation of CD4 cells - HIV's favorite target. An individual with inflammation from STDs who engages in unprotected sex has a higher risk of contracting HIV.
Wrong answers: The immune response to inflammation will not prevent HIV infection and it is incorrect to assume that someone with a sexually transmitted disease also has HIV.
How do you balance protecting yourself with not contributing to stigmatization of people living with HIV/AIDS by over-protecting yourself and making patients feel like they cannot be touched? Comment on our wiki using Moodle
The occupational risk of infection is low.
In Canada, there has been only one definite case of occupational transmission, and two probable cases.8
The best way for nurses to protect themselves from occupational exposure to HIV infection is to:
HIV has 2 protein surface receptors:
Video animation clearly showing HIV binding to CD4 cells.
The most detailed 3D model of HIV to date.
Recall that HIV is a retrovirus that carries RNA instead of DNA. Inside its cell membrane, it carries 2 strands of RNA and 3 viral enzymes.
HIV's 3 Viral Enzymes
Question: What 3 enzymes does HIV carry? Match the enzymes with its function.
Clinical Manifestations |
|
|
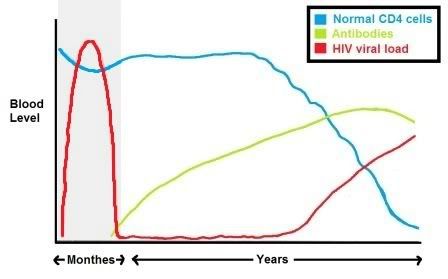
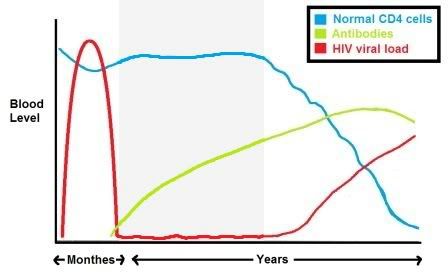
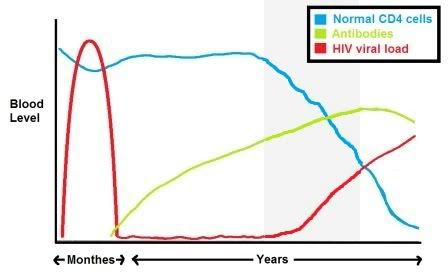
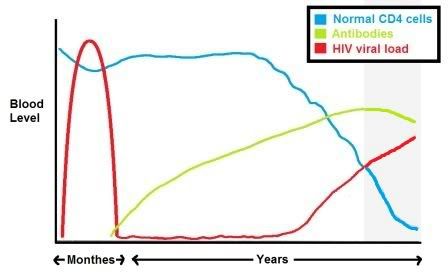
HIV Stage 1: Acute HIV Infection
Patients must wait for antibodies to develop (a process known as seroconversion) before HIV antibody tests will be accurate. This is known as the window period. Most people develop HIV antibodies within 6-12 weeks of infection. Research has shown that 95% of people who are infected with HIV develop antibodies within 34 days of the date of infection.13 Very rarely, it can take up to 6 months. The clinical manifestations of this stage resemble flu-like symptoms. Due to the non-specific nature of the signs and symptoms during this stage of HIV, diagnosis is often missed. Nurses play a role in helping to identify individuals at risk of contracting HIV and initiating HIV testing. Initial HIV infection resembles the flu:
Question: A patient is presenting with signs of the flu. During the history, the patient discloses engaging in recent unprotected sex with multiple partners. As his nurse, you recognize the increased risk of HIV from the engagement in risky behaviors and flu-like symptoms. An HIV antibody test is recommended and accepted by the patient. However, the results come back negative for HIV antibodies. What is your top priority for patient teaching? (Click one of the options below.)
|
|
HIV Stage 2: Asymptomatic stage
Clinical symptoms Treatment usually begins when the CD4+ cell count is less than 200 cells/mm3 |
|
HIV Stage 3: Symptomatic stage
Clinically: Co-trimoxazole has been used as a prophylaxis to prevent several HIV-related opportunistic infections (including TB, bacterial pneumonia, malaria, septicemia). Research has shown it to be effective in reducing deaths among individuals with HIV who are beginning treatment.14 |
|
HIV Stage 4: Progression of HIV to AIDS
Next Page: Etiology Back to main page Good job! #2 is correct. Sorry, wrong answer. Try again. :) Next Page: EtiologyBack to Main Page |
There is evidence that HIV originated from AfricaAfter HIV was first identified by the Centre for Disease Control in the United States, evidence emerged that indicated the HIV virus originated from monkeys in sub-Saharan Africa. HIV arises from the simian immunodeficiency virus (SIV), which shares significant genetic similarities to HIV and has only been found on the African continent1. There are 2 different strains of HIV: HIV-1 and HIV-2.
|
|
Co-infection with two or more different strains of HIV in an individual can occur which increases the likelihood of creating hybrids called circulating recombinant forms (CRFs).
Question 2: If two individuals are both HIV positive, do they need to use protection?Nurses play a role in providing education about treatment.
HIV/AIDS treatment begins with the provision of knowledge and information that can be used by patients as resource tools for make informed decisions regarding their treatment. Educating patients is the primary step in establishing a successful treatment plan.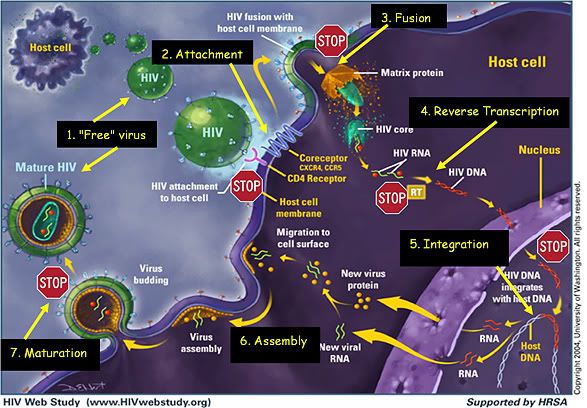
Nucleoside reverse transcriptase inhibitors (NRTI) function by inhibiting the enzymatic function of reverse transcriptase by binding to the polymerase active site of the reverse transcriptase enzyme of the HIV virus. In doing so, NRTI prevent the transcription of the virus's single stranded RNA into a double stranded DNA genome. The inability to produce new DNA strands interrupts thse production of new virons.
Non nucleoside reverse transcriptase inhibitors (NNRTI) operate by decreasing nucleoside incorporation rate by inducing structural modification of reverse transcriptase. NNRTI achieve this by binding to the hydrophobic pocket adjacent to the polymerase active site of reverse transcriptase as allosteric non competitive inhibitors.
Protease inhibitors (PI) function by inhibiting an enzyme known as Protease. Protease is responsible for cleaving large proteins into smaller structural proteins and reverse transcriptase, element required for the construction of a mature virus.
Integrase inhibitors function by inhibiting the integration of the HIV virus into the host cell.
Entry inhibitors operate by either inhibiting or antagonizing one of three main steps in the required for the entry of the HIV virus into the host cell.
These steps involve26:
Entry inhibitors are further subclassified into 3 categories based on the step of the viral entry process that they inhibit.
Maturation inhibitors are a potential new drug class which seeks to stop HIV particles from maturing after they have emerged from human cells. These drugs disrupt the final step in the processing of the HIV-1 Gag protein, leading to the formation of noninfectious, immature virus particles, incapable of infecting other cells. However, there are no currently available drugs from this class
"Nukes"Nucleoside Reverse Transcriptase Inhibitors |
"Non-nukes"Non-nucleoside Reverse Transcriptase Inhibitors |
Protease Inhibitors |
|
|
|
Integrase Inhibitors |
Fusion inhibitor |
Co-receptor Inhibitor |
Question: Match the drug(s) with its target (Click the drug names for a hint):
Things to keep in mind in regards to treatment
Resistance and Cross-resistance
Remember that HIV can also develop cross-resistance - that is, if one strain of HIV in an individual becomes resistant, similar strains will also have resistance to the same drugs.
"I became resistant to almost everything [in 2003]… We were waiting for a new drug called T-20. At one point my doctor pulled me off everything because the T-20 has to be taken in combination with other drugs, and if I’d stayed on all the drugs I would have become resistant to them all and the T-20 would have been useless." -Joe
Managing Side Effects
There are several options for dealing with side effects:In relation to HIV, alternative therapies are most commonly used in areas where it is difficult to access Western medicine. In the absence of antiretroviral treatment, people may seek other ways to delay the onset of AIDS, or to treat opportunistic infections. In sub-Saharan Africa, for example, traditional healers outnumber medically qualified doctors eighty-to-one22.
Because these treatments are so effective, there is less demand for alternative HIV medicine, except perhaps for addressing relatively minor infections, or when antiretroviral treatment cannot any longer be taken, for example because of drug resistance. Many instead look to complementary medicine as a way to prevent or relieve aids treatment side effects, some of which are not easily treatable with conventional medicine.
Interesting fact: In Gambia, the president himself has treated patients with a herbal mixture he claims is an AIDS cure. Analysis of data has not proven his "cure" to be effective, yet he continues to "treat" patients to this day.
There are also therapies that are not considered credible by the scientific community at large. The most notorious of these is homeopathy, which the World Health Organization recommends should not be used to treat HIV23.
St. John's wort is a popular herbal medicine for treating depression. It interacts with the liver and negatively interacts with anti-HIV drugs (protease inhibitors and NNRTIs). Patients taking ARVs should not take St. John's wort.
|
Calanolide A, an isolated compound from a type of tree, has been found to act like ARVs, more specifically to be a naturally occurring non-nucleoside reverse transcriptase inhibitor (NNRTI). It has been found to be effective against some strains of HIV that had become resistant to other ARVs24,25. It is thought to work by binding to 2 sites on the reverse transcriptase enzyme of HIV. |  |
KEY MESSAGE: Support patients in taking control of their own healthcare decision-making. Nursing role is to provide information so that patients can make informed decisions.
Back to top